P. vivax liver stage treatment
P. vivax liver stage malaria treatment: primaquine & tafenoquine
Until recently, primaquine was the only option for P. vivax liver-stage treatment. In 2018, with the regulatory approval of tafenoquine (a primaquine analogue with a long half-life), there is an alternative. Both drugs are 8-aminoquinolines and need to be given with an appropriate blood stage drug to achieve radical cure.
Primaquine
Primaquine is the WHO-recommended treatment for relapse prevention at an adult dose of 15 mg/day for 14 days in areas where P. vivax temperate strains predominate . Additionally, the WHO advises treatment of 30 mg/day for 14 days where rapidly relapsing tropical strains are prevalent.1
Two primaquine products are manufactured to international standards and are WHO prequalified. Both are on the current Global Fund list of approved malaria pharmaceutical products. Tablets are available at 7.5 mg (Remedica) and 15 mg (Sanofi/ Valeant Pharmaceuticals) as base. More information on the dose calculation per patient body weight for primaquine may be found from the World Health Organisation's treatment guidelines for malaria.
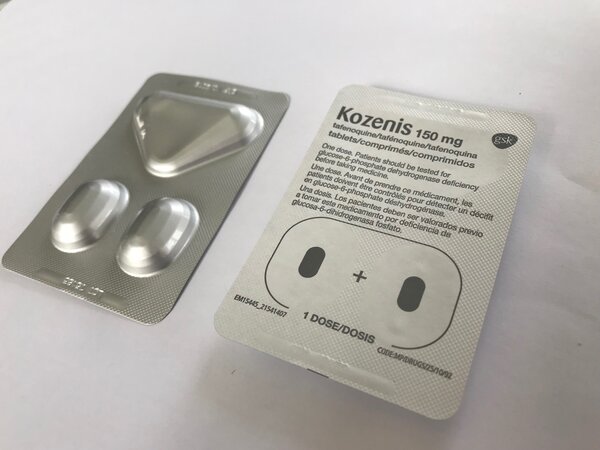
Tafenoquine
Tafenoquine, a single dose liver-stage treatment, has been shown to reduce P. vivax relapse by around 70% versus placebo.2 The convenience of this regimen as a single-dose regimen reduces the risk of low or non-compliance.
At present tafenoquine, manufactured by GlaxoSmithKline, is licensed for use with chloroquine and studies are being conducted for combination with ACTs.
Medicines for Malaria Venture (MMV) provide up-to-date information on the registration status of tafenoquine worldwide.
Restrictions of use for primaquine and tafenoquine
Primaquine
- Primaquine cannot be given to pregnant women, infants aged less than 6 months, women who are breastfeeding an infant aged less than 6 months, or women breastfeeding older infants who are G6PD deficient (or whose G6PD status is unknown).
- Primaquine also requires metabolic conversion to the active metabolite and efficacy is impeded in individuals with a slow CYP2D6 metaboliser phenotype.1 This phenotype is common in many P. vivax endemic countries.
Tafenoquine
- Tafenoquine is also contraindicated in infants, pregnant women and women who are breastfeeding an infant whose G6PD status is unknown or who is G6PD deficient.
- Tafenoquine, like primaquine, causes dose-dependent haemolysis in individuals who are glucose-6-phosphate dehydrogenase deficient (see G6PD deficiency). WHO recommends a weekly primaquine dose for G6PD deficient subjects (at 0.75 mg/kg per week for 8 weeks) provided that medical supervision is available, and the patient has access to safe blood transfusion facilities.
- As tafenoquine is a single-dose therapy, treatment cannot be stopped or divided. Thus, G6PD testing with a quantitative G6PD test is mandatory to ensure that is only given to individuals with greater than 70% enzyme activity.
- Since tafenoquine does seem to require metabolic conversion to an active form, efficacy is probably unaffected by CYP2D6 phenotype.3

Opportunities for the wider administration of radical cure
The expansion of access to P. vivax radical cure not only has the potential to reduce malaria burden but also to reduce transmission and accelerate malaria elimination.
Mathematical modelling indicates that relapse prevention through mass drug administration (MDA) with primaquine in conjunction with G6PD testing could result in substantial reductions in P. vivax transmission.
However, the operational barriers to delivering supervised primaquine are considerable.4 In contrast, mass screen and treat (MSAT) would be ineffective, as hypnozoite carriers cannot be identified and would, therefore, continue to experience relapses and transmit malaria.
A mathematical model constructed for Papua New Guinea indicated that first-line treatment with primaquine or tafenoquine for symptomatic P. vivax cases would further reduce transmission in areas with enhanced vector control measures, and that the greatest reduction in transmission would occur in areas that continued to have high transmission even after the deployment of vector control.5, 6
With the availability of single-dose tafenoquine and improved G6PD point-of-care diagnostics, field evaluation of the impact of 8-aminoquinolines on P. vivax transmission becomes more feasible. Data could also be generated to refine existing mathematical models indicating the most effective deployment strategies for G6PD deficiency diagnostics.